Work and health are inextricably linked – and can have both positive and negative impact on each other, says Clare Forshaw, Occupational Health & Hygiene Partner at Park Health & Safety.

Clare Forshaw
Most of us by now acknowledge the evidence that points to good work being good for us. Waddell and Burton’s influential review Is work good for your health and wellbeing (2006) concluded that work is generally good for physical and mental health and well-being and can be therapeutic for people with common health problems. Also that for individuals with common health conditions (mental health, cardio-respiratory and musculoskeletal condition) consensus holds that – for the good of their health – they should remain in, or return as soon as possible to, work.
When it comes to the wide scope of ‘health’ of the workforce and what is expected of employers the topic can become a huge headache and this means it often ends up in the ‘too difficult’ box.
Common health problems
There are a number of health issues that face our workforce and as health and safety professionals we are used to dealing with health risks created by the work tasks themselves. Employers and health and safety professionals also like to be able to clearly identify health issues CAUSED by work and those not, so that we can clearly distinguish and deal with each separately. However, with some common workplace health issues this is difficult, if not often impossible, to do.
These can be termed ‘common health problems’ and can be considered of increasing importance in terms of impact as they tend to be the most prevalent and stubborn problems for both individuals, businesses and society. These health issues occur most commonly across the population, contribute most significantly to long term sickness absence and can affect productivity, safety and accidents at work.
Common Health Problems are invariably related to musculoskeletal problems (including back pain, neck, and upper limb problems), mental health and stress.
What makes these health issues particularly problematic for employers and health professionals is founded in a number pertinent issues;
- They are often subjective and variable in terms of symptoms – making diagnosis and prognosis difficult;
- They are multifactorial – many different issues/exposures combine to result in an unpredictable health outcome;
- They often coexist – so people with MSDs often suffer a mental health issue;
- They can be influenced by both work and non-work factors – however they can be termed ‘work relevant’ due to the impact seen and felt at the workplace.
These issues combine to make any preventative actions difficult and treatment uncertain. However, considering the scale and impact these health issues have, the likelihood is that with an ageing workforce, skills shortages and retention issues the problem is only likely to get bigger!
Cost of sickness absence
The fact is that we have over 75% of adults in Great Britain in employment (the highest proportion since records began), on average spending a third of their waking hours in the workplace. The annual costs of sickness absence to employers is on average £16 billlion and over 137 million days were lost to sickness absence in the UK in 2016 (HSE). 22% of sickness absences are caused by musculoskeletal conditions and 11.5% as a result of mental health issues (including stress, depression and anxiety) (ONS 2016).
According to the CIPD the average recruitment cost of filling a vacancy is £4,000, increasing to £6,125 when the associated labour turnover costs are included. Another quote puts the cost at over £30K taking into account the time needed to get up to speed with the job!
So how can we better tackle these ‘common health problems’ and what role can health and safety professionals contribute? Firstly, we need to overcome the hang-ups of whether these issues were caused by work or not – the term ‘work relevant’ sums up the imperative to address the problem at the workplace. Also, we can acknowledge the wide evidence base that demonstrates that there are certainly common workplace exposures that WILL cause, contribute and affect MSD’s and mental health.
Secondly, we need to look beyond our traditional approaches of risk management and health interventions (treatments) as they have proved ineffective in either identification or resolving these matters.
Our traditional workplace approach to risk management is difficult to apply to common health problems because the usual approach relies on an understood level of risk and related response that produces an outcome which is readily identified. When it comes to common health problems they can be caused by an unidentifiable accumulation of ‘exposures’ – both work-related and non-work related and are also affected by individual factors.
Also due to the recurrent and variable nature of symptoms and impact on individuals a traditional medical model often fails.
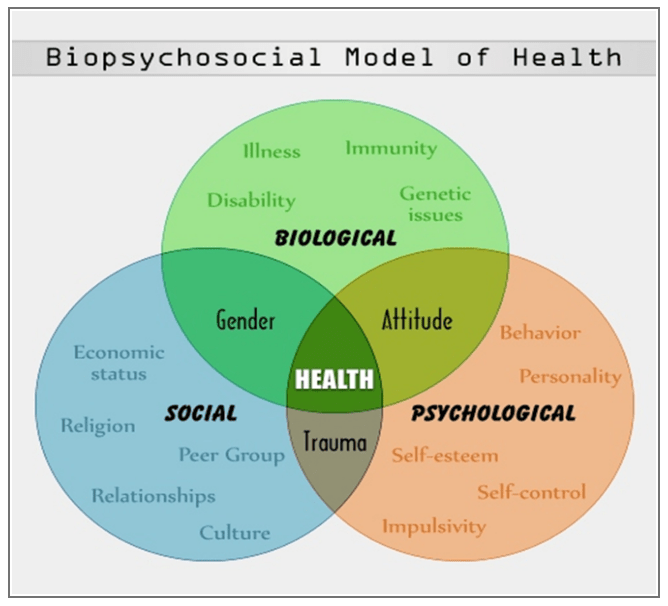
A biopsychosocial model approach best suits these issues in that it takes account of the much broader intricate and variable interaction of biological (genetic, biochemical, etc), psychological (mood, personality, behaviour, etc.), and social factors (cultural, familial, socioeconomic, medical, etc).

We also need improved acknowledgment and ownership of common health problems in the workplace in order to move forward. We can apply better work organisation and improved quality of management principles – the two L’s for me are key to making the difference – Leadership and Line Management.
Having a healthy and productive workforce is more important today than ever. Employers need to provide good work, good jobs and supportive workplaces when people fall ill. A safe workplace is an essential element to this but health and safety professionals can also contribute to identifying and quantifying common health issues in the workforce. These professionals can manage the workplace risks for MSD and mental health and contribute to risk assessments for individuals who have ‘work relevant’ conditions. We need to move forward and better engage our workforce on these matters and improve our systems and procedures to positively affect the occurrence and impact of common health issues and keep people healthy, happy and at work.
Clare will be speaking on this topic at the European HSE Management Forum in Amsterdam 20 – 21 September.
What makes us susceptible to burnout?
In this episode of the Safety & Health Podcast, ‘Burnout, stress and being human’, Heather Beach is joined by Stacy Thomson to discuss burnout, perfectionism and how to deal with burnout as an individual, as management and as an organisation.
We provide an insight on how to tackle burnout and why mental health is such a taboo subject, particularly in the workplace.



Easy peasy, human stress levels can be objectively and instantly, well 90 seconds, measured, as there is a direct correlation between their heightened anxiety state driven by their fight-flight response manifesting in the stimulation of stress hormones (HPA Axis) and as a result calculable deficits in capacity to sustain stable binocular vision in terms of accommodation and vergence. Of course, this can also be historically established by a path-lab analysis of bodily fluids, saliva, blood or urine samples but, that requires time to take, send off and process before you get the results. The same would apply to a longitudinal… Read more »